AMPUTATION AND AMPUTATION SURGERY
vascular.co.nz>amputation surgery
What is an amputation?
Why do patients need to undergo amputations?
What sort of amputations can be performed?
How will having an amputation affect me?
What are the risks of amputation surgery?
What are the complications of amputation surgery?
Is it possible to walk after an
amputation?
What will happen after my
amputation?
References
Useful names and addresses
Amputation links
What is an amputation?
An amputation usually refers to the removal of the whole or part of an arm/hand or a leg/foot. Amputations can occur after an injury (traumatic amputation) or deliberately at surgery. In vascular surgery amputations are only rarely performed on the arms. Vascular surgeons frequently have to perform amputations of toes or legs. It is one of the oldest surgical procedures with artificial limbs identified from over 2000 years ago.
Why do patients need to undergo amputations?
The vast majority of amputations are performed because the arteries of the legs have become blocked due to hardening of the arteries (atherosclerosis). Blockages in the arteries result in insufficient blood supply to the limb. Because diabetes can cause hardening of the arteries, about 30-40% of amputations are performed in patients with diabetes. Patients with diabetes can develop foot/toe ulceration and about 7% of patients will have an active ulcer or a healed ulcer. Ulcers are recurrent in many patients and approximately 5-15% of diabetic patients with ulcers will ultimately require an amputation. Because hardening of the arteries occurs most commonly in older men who smoke, the majority of amputations for vascular disease occur in this group. Diabetes may be an important factor in nearly 40% of patients undergoing major amputation (Moxey et al 2010).
When hardening of the arteries becomes so severe that gangrene develops or pain becomes constant and severe, amputation may be the only option. If amputation is not performed in these circumstances infection can develop and threaten the life of the patient. Sometimes bypass surgery can be performed to avoid amputation, but not all patients are suitable for bypass surgery. Before amputation, the limb can cause serious problems with infection and pain and may even be a threat to the life of some patients.
Less commonly serious accidents can lead to the loss of a limb, as can the development of a tumour or cancer in a limb. These amputations tend to occur in younger patients.
About 370 new referrals are made to the NZ artificial limb board annually of which about 300 (70%) are due to vascular causes and diabetes. Over the period 2003-2008 in the UK there were approximately 5 major amputations (above or below knee) per 100,000 people (Moxey et al 2010).
What sort of amputations can be performed?
Amputations can be divided into minor and major. Most vascular surgeons will have extensive experience in this type of surgery.
Minor amputations are amputations where only a
toe or part of the foot is removed. A ray amputation is a particular form of
minor amputation where a toe and part of the corresponding metatarsal bone is
removed as shown in the diagram below left. A forefoot amputation can
sometimes be helpful in patients with more than one toe involved by gangrene.
In this operation all of the toes and the ball of the foot is removed.
Major amputations are amputations where part of the leg is removed. These are usually below the knee or above the knee.
Occasionally an amputation of just the foot can be performed with a cut through the ankle joint (Symes amputation). This is not suitable for the majority of patients, but can rarely be an option in some patients with diabetes. It is particularly important for this amputation that the posterior tibial artery is patent and has a reasonable blood flow. This artery is found on the inside of the foot just below the ankle. Your surgeon may advise you if this operation may be possible.
Amputations through the knee joint or just above the knee joint (Gritti-Stokes amputation) can also sometimes be performed. They were much more popular amputations in the past but there is little or no advantage for present day patients compared with above knee amputation. If a major amputation is to be performed then a below knee amputation will always give the patient the best chance of remaining mobile and walking post-operatively.
Minor amputations
After minor amputations the wound is not always closed completely with stitches. If infection is present or too much skin has had to be removed then the surgeon may leave the amputation wound open. When a ray amputation is performed the wound is usually left open to heal. This sounds awful and to the untrained eye the resulting wound can appear dreadful. If the wound is open do not be disheartened. If the conditions are right for healing these wounds can heal well over a period of 1-3 months and leave a fully functioning leg and foot. It is possible to walk virtually normally after losing toes. Even after a forefoot amputation where all the toes are removed, walking is usually straightforward.
This sort of operation is performed frequently for foot infections in patients with diabetes.
Major amputations
It is usually possible before the operation (although not always) for the surgeon to decide at what level the amputation will be performed (above knee or below knee). Sometimes gangrene or infection will only involve a toe or part of a foot and a limited or minor amputation can be performed. This is only worthwhile if the surgeon thinks that the wound that is created will heal. In some patients, it is better to try a limited amputation if there is a chance of healing, but to be prepared to proceed to a major amputation if healing doesn't take place.
One of the most important factors in healing is the blood supply to the tissues. If the blood supply is damaged or impaired it may not be possible for the tissues to heal even after a minor amputation. If in the opinion of the surgeon the tissues will clearly not heal because of a poor blood supply it would be reckless to proceed with a minor amputation when really a major amputation is required. Unfortunately, there is no test that can predict in every patient whether healing will take place and it is a matter of surgical judgement and experience whether a wound is likely to heal or not.
In general the more limited the amputation the lower the risks and the better the chances of walking. It is better to have a below knee amputation when compared with an above knee amputation, because the chances of successfully walking after the operation are much better. Unfortunately, not everyone is suitable for this operation and many people need to have an above knee amputation. This may be because the blood supply to the lower leg is too poor and a below knee amputation would not heal properly. If the knee cannot straighten out properly before the surgery (fixed flexion deformity), it will be impossible to walk with an artificial leg after the operation. In these circumstances it may be better to undergo an above knee amputation.
Once an amputation stump is created it is a potentially vulnerable area that will require lifelong care and attention. A major amputation wound is almost always closed with stitches or staples. A major amputation will take approximately 60-90 minutes to perform. Small plastic tubes are often inserted into the stumps before the end of the operation. These are drains which are used to take away any excess fluid that accumulates in the wounds. They are usually removed in the first 48 hours.
Below knee amputation
This operation can be performed using 2 major
techniques. The most common technique is the posterior myoplastic flap (Burgess technique) where the skin and muscle from the calf are brought forward to cover the shin bones after they have ben divided (see below left). The other main technique is the skew flap (Kingsley Robinson technique) in which the muscles of the calf are brought forward in the same way as in the posterior technique but the skin flaps are skewed in relation to the muscle. There is no proven advantage
for one technique, but sometimes it is easier to perform a skew flap amputation
if there has been significant skin damage above the ankle. The bone in the
lower leg (tibia) is divided about 12-15 cms below the knee joint. This produces a good size stump to which a prosthesis can be fitted.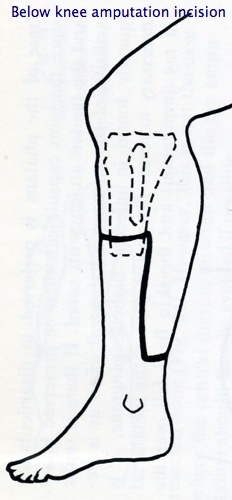
Above knee amputation
In this operation the bone in the thigh (femur) is divided about 12-15 cms above the knee joint and the muscle and skin closed over the end of the bone.
If you wish to see an amputation being performed a short search of the internet will provide many video examples - see here.
How will having an amputation affect me?
Amputation of a limb or limbs will affect people in different ways. It is a very personal loss and in many patients can feel like a bereavement. The emotional loss can be like losing a relative and it will take time to adapt to such a loss. Physically your body will be permanently altered and can affect all areas of your life. How much your amputation affects your life will to some degree depend on the extent of your physical recovery.
There are virtually no activities that a person with an amputation cannot perform with the right help, training and equipment. However, the most important rehabilitation objective for the majority of elderly patients with a lower limb amputation is to walk again. It is important to remember that rehabilitation from an amputation in an elderly person is a much more difficult process than in a young person. Regaining the ability to walk will be a major achievement.
Whether or not a patient will be able to walk following an amputation has been studied by looking at factors present before surgery. Poor pre-operative mobility, age over 70 years, dementia, severe kidney and heart disease are factors which make it unlikely a patient will walk after their amputation (Taylor SM et al, 2005).
What are the risks of amputation surgery?
There are significant risks attached to undergoing an amputation if you are elderly and have hardening of the arteries. In this group of patients the chances of dying in hospital after a major amputation are somewhere between 10% and 20%. In other words between 1 in 10 and 1 in 5 patients, undergoing a major amputation for hardening of the arteries, will die in hospital. This is why amputation is always a last resort and your surgeon will not advise you to undergo this operation unless it is absolutely necessary. Remember these statistics also mean that 4 out of 5 patients undergoing an amputation will do well.
If you are younger and healthy and undergo amputation because of an injury or a tumour, the risks of an amputation are usually much less.
In a UK study examining amputations over the previous 5 years the overall chance of dying from an above knee amputation was 21.4% and was 11.6% for a below knee amputation (Moxey et al 2010). For minor amputations there was a 3.6% risk of dying.
What are the complications of amputation surgery?
The most important complication is the risk of dying. However, there are other complications.
General complications
These mainly consist of problems such as chest infections, angina, heart
attacks and strokes. Because your mobility is restricted after an
amputation, pressure sores can also develop. The nursing staff particularly
will make great efforts to avoid this occurring. Special mattresses and
beds are used to reduce pressure on areas at risk of sores. Regular
turning to relieve pressure is also important.
Local complications
These mainly consist of wound infections that can develop in the stump.
Antibiotics are given to reduce the risk of infection developing at the time of
surgery. The stump can sometimes fail to heal or breakdown either as a result of a fall,
infection or a poor blood supply. When this happens it can sometimes mean
a further operation to revise the amputation or to remove more of the leg.
Sometimes contractures can develop in the knee or hip joint and once present and established can be impossible to correct. The knee or hip will not straighten and then fitting an artificial limb can become impossible. Physiotherapy to keep the joints supple will begin almost immediately after the operation to avoid the risk of contracture.
Deep venous thrombosis can also occur because the veins in the leg will have been tied during the amputation operation and because of the immobility after the surgery. Blood thinners (heparin) will usually be given to reduce the risk of blood clots developing.
Phantom Limb pain
Phantom limb is the sensation of still being able to feel the amputated limb.
Most amputees experience this sensation, although the intensity can vary from
person to person.
In many patients pain is also experienced in the amputated limb. This is phantom limb pain and can occur in many patients, but is usually fairly mild and self limiting, although it may be a nuisance. In a few patients phantom limb pain can be a serious problem and difficult to treat.
Is it possible to walk after an amputation?
Yes, it is possible to walk after an amputation. How easy it will be to walk depends on a number of factors. For instance it is generally easier to walk with an artificial leg (prosthesis) after a below knee amputation. If you were able to walk normally before your amputation and do not have other illnesses such as angina or breathing difficulties this will also make it more likely you will walk after your amputation.
Some studies have shown that in elderly patients undergoing major amputation (below or above knee) for hardening of the arteries, over half the patients fitted with an artificial leg never used it effectively, especially if rehabilitation was delayed for longer than two months after the amputation. It can take between 6 and 12 months for full rehabilitation potential to be reached.
Most patients undergoing minor amputation will be able to walk virtually normally after surgery.
What will happen after my amputation?
Initially there will be a period of recovery from the operation. Once recovery from the surgery has taken place, physiotherapists and occupational therapists will concentrate on enabling you to manage independently. This will require learning new skills, such as moving from a wheelchair to the bed and back again, using a wheelchair and starting to use an artificial limb. There will be various exercises to strengthen the upper body and maintain flexibility and movement in the amputated leg.
If you are well enough it may be possible to walk on a temporary artificial leg (PAM aid, pneumatic aid to mobilisation) very soon after your operation. This prosthesis has an inflatable section which is placed around the newly formed stump. This can be a very successful method of early rehabilitation, but a permanent made-to-measure artificial leg will be made for you after referral and assessment at the local limb fitting centre. This can only be done when your leg swelling is getting better and may take more than one attempt before the right fit is obtained.
After an amputation the majority of patients need the help of a wheelchair to remain mobile. Sometimes the use of a wheelchair may be the best way of remaining mobile. If you are very elderly or have had other serious illnesses such as heart disease or stroke then it can frequently be better not to be fitted with an artificial leg.
Amputation links
![]() Bookmark this on Delicious
Bookmark this on Delicious  reddit
reddit 
![]() facebook
facebook
Taylor SM, Kalbaugh CA, Blackhurst DW et al. Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg 2005; 42: 227-35.
Moxey PW, Hofman D, Hinchcliffe RJ, Jones K, Thompson MM, Holt PJE. Epidemiological study of lower limb amputation in England between 2003 and 2008. Brit J Surg 2010; 97: 1348-1353.
Amputee Federation of New Zealand (Inc)
http://www.amputee.co.nz/
New Zealand Artificial Limb Board
International Society of Prosthetics and
Orthotics (ISPO)
Dept Mechanical Engineering, Univ College London, Torrington Place, London WC1E
7JE
Limbless Association
31 The Mall, Ealing, London W5 2PX UK. Tel 00 44 (0)181 579 1758
Last updated> 27 August, 2010